Sepsis kills 350,000 Americans annually, yet 4–8% more die for every hour treatment is delayed. Machine learning algorithms can detect it hours earlier than clinicians—and evidence shows they save lives. So why aren’t they everywhere?
The Algorithm Advantage
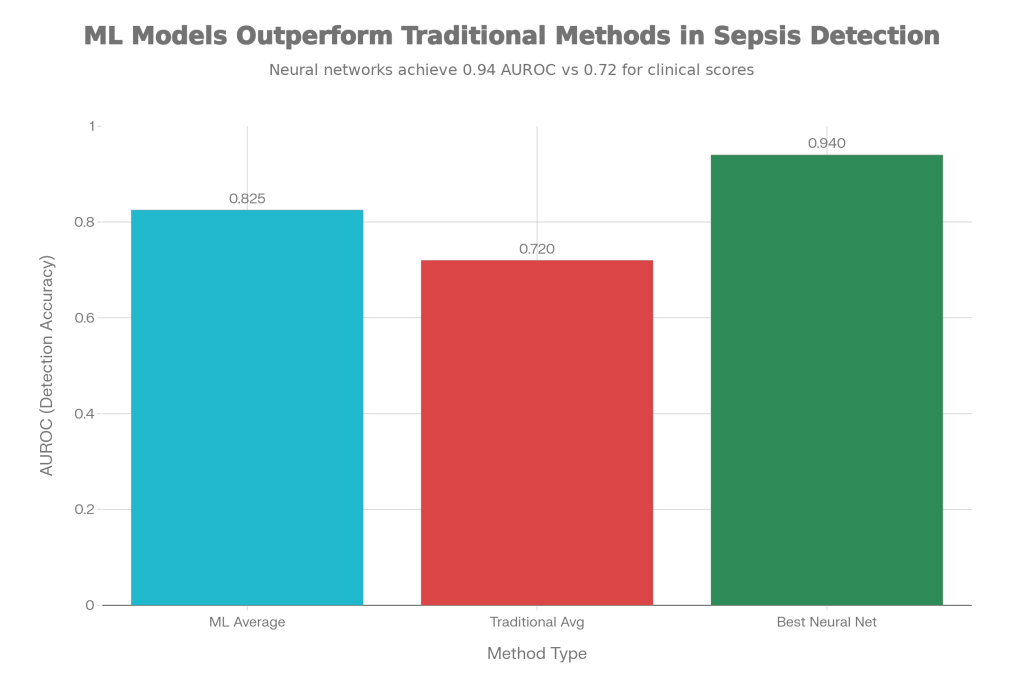
Machine learning models dramatically outperform traditional clinical scoring systems. A 2024 meta-analysis of 73 studies found ML algorithms achieve 0.825 accuracy (AUROC) versus 0.72 for traditional methods like qSOFA and SIRS. Top neural networks reach 0.94 accuracy.
More importantly, when deployed clinically, they work. A 2024 prospective study at UC San Diego Health tracked 6,217 sepsis patients and found algorithm-assisted care reduced mortality by 17% (9.49% versus expected 11.39%). A separate multi-hospital study reported even larger mortality reductions of 39.5%. Antibiotics were administered 30–40 minutes faster when algorithms flagged at-risk patients.
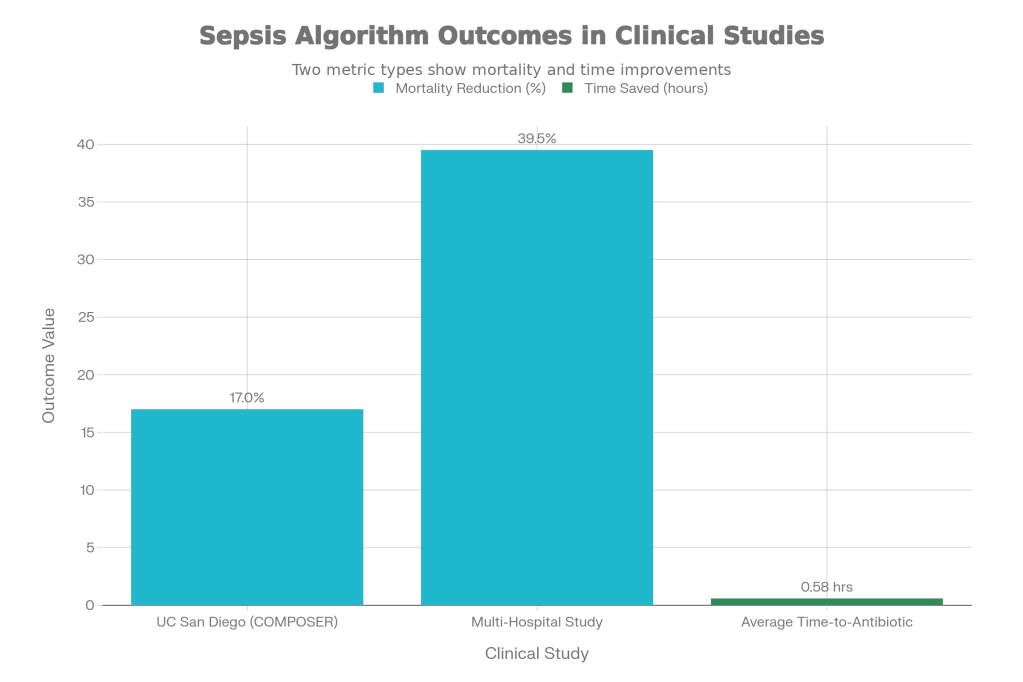
For a typical hospital with 200 sepsis admissions yearly, a 17–20% mortality reduction means 3–6 fewer deaths annually. Yet adoption remains sparse.
Why Hospitals Aren’t Using Them
The Implementation Gap: A 2020 systematic review found that of 28 sepsis prediction papers published, only 3 (11%) achieved clinical implementation. That’s the research-to-practice valley.
Alert Fatigue: Traditional sepsis alerts fire constantly—in roughly 40% of patients who don’t have sepsis. Clinicians stop responding. Modern algorithms like SepsisAI reduce false alarms to 3%, but most hospitals still use older systems. This single factor explains much of the adoption barrier.
Heterogeneous Definitions: Sepsis looks different across patients and institutions. Respiratory infections, urinary tract infections, and intra-abdominal infections trigger sepsis through different mechanisms. Inconsistent definitions across hospitals make it hard for algorithms trained in one setting to work in another.
Workflow Integration: Algorithms exist in isolation. An alert appears in the EHR, but without clear protocols—Who sees the alert? What action triggers?—it becomes noise. In the UC San Diego study, mortality benefits only appeared when nurses actively escalated alerts to physicians.
The implementation gap: Research exists, but clinical adoption remains low, and false alarm reduction hasn’t yet driven widespread use

Where It Actually Works
Emergency departments show the most consistent results. They’re high-volume settings with time pressure and rapid triage needs—precisely where an algorithm providing early risk ranking adds clear value. When sepsis alert systems integrate with rapid response teams and standardized treatment bundles, outcomes improve.
The Opportunity
The evidence is clear: algorithms can reduce sepsis mortality when thoughtfully deployed. But success requires:
- Reducing false alarms through advanced warning systems
- Integrating alerts into actual workflows with clear action protocols
- Standardizing sepsis definitions across institutions
- Building clinician trust through explainability
- Conducting prospective trials in diverse hospital types
We have the technology. The gap is implementation—organizational change, staff training, and commitment to translating research into routine practice. Until that happens, lives will continue to be lost despite having the tools to save them.
References
Gupta A, et al. Improving sepsis prediction in intensive care with SepsisAI: A clinical decision support system with focus on minimizing false alarms. PLOS Digital Health. 2024.
Frontiers in Medicine. Early detection of sepsis using machine learning algorithms: a systematic review and network meta-analysis. 2024.
Shashikumar SP, et al. Advanced meta-ensemble machine learning models for early and accurate sepsis prediction. 2024.
Boussina M, et al. Impact of a deep learning sepsis prediction model on quality of care and survival. Nature Digital Medicine. 2024.
Kim H, et al. Sepsis alert systems, mortality, and adherence in emergency departments. JAMA Network Open. 2024.
Fleuren LM, et al. Machine learning for the prediction of sepsis: a systematic review and meta-analysis. Intensive Care Medicine. 2020.
Leave a comment